Possible Complications
A damaged liver affects almost every bodily process, including the functions of the digestive, hormonal, and circulatory systems. Decompensated cirrhosis increases the risk of serious and potentially life-threatening complications. (Once decompensation occurs, mortality rates without liver transplantation can be as high as 85% within 5 years.) The most serious complications are those associated with portal hypertension (increased pressure in the portal vein that carries blood from the intestine to the liver). They include:
- Ascites (fluid buildup in the abdomen)
- Variceal hemorrhage (bleeding in the upper stomach and esophagus from ruptured blood vessels)
- Spontaneous bacterial peritonitis is a form of peritonitis (inflammation of the membrane that lines the abdomen), which is associated with ascites. Other bacterial infections are also a common complication of cirrhosis.
- Hepatic encephalopathy (damage to the brain). Impaired brain function occurs when the liver cannot detoxify harmful substances, and can lead to coma.
Liver cancer is a serious long-term risk with cirrhosis. Other complications also occur.
Diagnosis
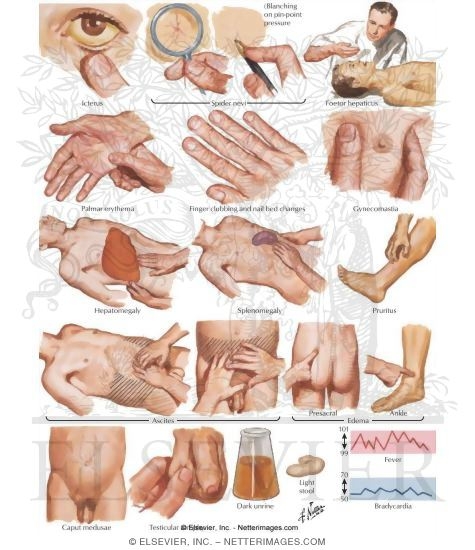
A physical examination may reveal the following in a patient with cirrhosis:
- The cirrhotic liver is firm and often enlarged in early stages of the disease. The liver may feel rock-hard. (In advanced stages of cirrhosis, the liver may become small and shriveled.)
- If the abdomen is swollen, the doctor will check for ascites by tapping the flanks and listening for a dull thud and feeling the abdomen for a shifting wave of fluid.
- The doctor will also check for signs of jaundice, muscle wasting, and (in male patients) breast enlargement.
A patient’s medical history is another indicator of the risk for cirrhosis. Patients with a history of alcoholism, hepatitis B or C, or certain other medical conditions are at high risk.
Other tests (blood tests, imaging tests, liver biopsy) may also be performed. The results of these tests along with the presence of specific complications (ascites and encephalopathy) are used for calculating the Child-Pugh Classification. This is a staging system (A to C) that helps doctors determine the severity of cirrhosis and predict the development of future complications.